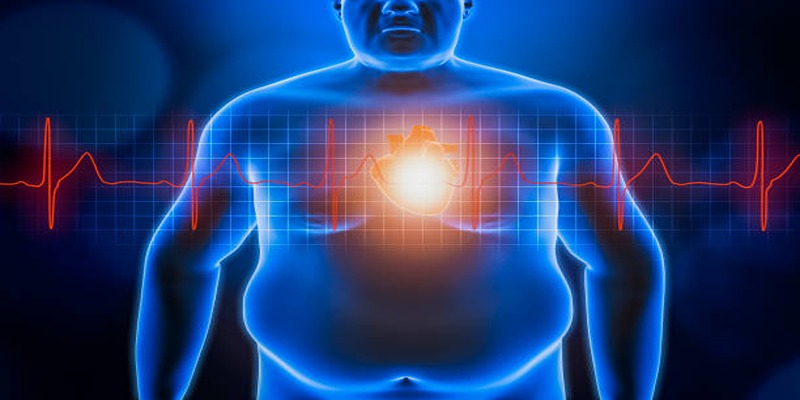
Excess Belly Fat Tied to Higher Heart Disease Risk
Excess fat around the belly is more than a mere aesthetic issue—it's a primary sign of possible health hazards, especially heart disease. Studies have established that the storage of visceral fat around the midsection considerably increases the risk of cardiovascular disease. This article will discuss the relationship between belly fat and heart health, describe the underlying risks, and offer practical advice on how to control and decrease abdominal fat for a healthier heart and general well-being.
Relationship between belly fat and heart disease
The connection between belly fat and heart disease is due to the fact that visceral fat, which is stored deep in the abdomen and covers essential organs like the liver and intestines, releases toxic substances into the body. These substances, such as free fatty acids, cytokines, and hormones, have been associated with inflammation, insulin resistance, high blood pressure, and other risk factors for heart disease.
Causes of Excess Belly Fat
Excess fat around the stomach can occur due to a number of causes, from bad lifestyle habits to genetic predispositions. The following are some prominent contributors:
Poor Diet Choices

A diet rich in processed foods, added sugars, and poor fats can cause weight gain and rise in abdominal fat. These foods tend to be calorie-rich but nutrient-poor, thus creating an imbalance between the supply and use of energy. Also, sweetened drinks such as sodas are a source of empty calories and major contributors to fat storage around the belly.
Lack of physical activity
Physical inactivity is one of the leading causes of extra belly fat. Without constant activity, the body cannot burn consumed calories, resulting in weight increase over time. Physical inactivity can also dampen metabolism, making it increasingly difficult to lose fat. Including regular exercise like cardiovascular exercise and strength training can greatly lower belly fat and increase overall metabolism.
Stress and Cortisol Levels
Chronic stress triggers the release of cortisol, a hormone that plays a role in fat storage, particularly in the abdominal area. High cortisol levels encourage the body to store fat around the belly as a response to perceived threats. Stress also promotes unhealthy coping mechanisms, such as overeating or consuming comfort foods, further exacerbating weight gain and belly fat issues.
Genetics and Hormonal Changes
For some individuals, genetic predisposition plays a significant role in the distribution of body fat, including around the abdomen. Hormonal changes, such as those during menopause, may also contribute to fat accumulation in this area. Genetics and hormones can influence metabolism, appetite, and weight distribution, making some people more prone to gaining belly fat than others, despite maintaining a healthy lifestyle.
Connection Between Belly Fat and Heart Disease
Belly fat is not just a cosmetic concern—it plays a critical role in affecting overall health and increasing the risk of heart disease.
Role of Visceral Fat in Increasing Cardiovascular Risk
Visceral fat, the fat stored deep within the abdominal cavity around vital organs, is particularly harmful. It releases inflammatory markers and hormones that disrupt the body's normal functioning. This type of fat increases the risk of atherosclerosis, a condition that narrows the arteries. Over time, it puts significant strain on the cardiovascular system, contributing to heart disease, heart attacks, and strokes.
Impact on Cholesterol Levels and Blood Pressure
Excess belly fat can negatively affect cholesterol levels by increasing low-density lipoprotein (LDL), often known as "bad" cholesterol, and reducing high-density lipoprotein (HDL), the "good" cholesterol. Additionally, visceral fat leads to higher blood pressure levels due to the release of substances that affect blood vessel function. These changes compound the strain on the heart, progressively raising the risk of cardiovascular events.
Influence on Inflammation and Insulin Resistance
Belly fat contributes to chronic inflammation by releasing pro-inflammatory cytokines, which affect the immune response and damage tissues. This persistent low-grade inflammation is a key factor in many chronic diseases, including heart disease. Furthermore, visceral fat impairs the body's ability to use insulin effectively, leading to insulin resistance. This condition increases the risk of type 2 diabetes, which further exacerbates cardiovascular health risks.
Health Complications

Belly fat is linked to many health issues beyond heart disease, including type 2 diabetes. Excess visceral fat promotes insulin resistance, where cells don’t respond properly to insulin, leading to high blood sugar and, over time, diabetes. If untreated, this can cause complications like kidney damage, nerve issues, and vision problems.
Belly fat is also tied to metabolic syndrome—a combination of high blood pressure, high blood sugar, abnormal cholesterol, and excess abdominal fat—which increases the risk of stroke and liver disease. Additionally, belly fat is linked to some cancers, like colorectal and breast cancer, due to the chronic inflammation it causes.
The effects of belly fat go beyond physical health, impacting quality of life. Chronic inflammation and hormone imbalances can cause fatigue and lower energy, while reduced self-esteem and higher stress may worsen overall health. Tackling belly fat through a healthy diet, regular exercise, and stress management is key to avoiding these complications.
Preventive Measures
Adopting effective preventive measures can significantly reduce belly fat and its associated health risks. Focus on the following strategies:
- Maintain a Balanced Diet: Include whole foods, high-fiber vegetables, lean proteins, and healthy fats while avoiding excess sugar and processed foods.
- Stay Physically Active: Engage in regular aerobic exercises like walking, jogging, or swimming, along with strength training.
- Prioritize Sleep: Strive for 7–8 hours of restful sleep each night to support balanced hormone regulation, particularly those tied to appetite and stress.
- Manage Stress: Practice stress-reduction techniques such as meditation, yoga, or deep breathing to lower cortisol levels.
- Stay Consistent: Adopt sustainable lifestyle habits instead of seeking quick fixes.
Treatment Options
Treatment options for weight management vary depending on individual needs and medical guidance. Below are some common approaches:
- Behavioral Therapy: Working with a counselor or therapist to develop healthy habits and address emotional eating.
- Medications: Using doctor-prescribed medications to aid weight loss when lifestyle changes alone are insufficient.
- Surgical Options: Considering procedures such as gastric bypass or sleeve gastrectomy for those with severe obesity.
- Medical Nutrition Therapy: Consulting a dietitian to create personalized meal plans that support weight goals.
- Group Support Programs: Joining structured programs that provide accountability and peer support.
- Technology-Assisted Tools: Utilizing apps and wearable devices to monitor activity and calorie intake.
Conclusion
Maintaining a healthy weight is a lifelong commitment that requires a balanced approach combining diet, exercise, and mental well-being. While various treatment options exist, it is essential to choose methods that align with individual needs and are guided by medical professionals. Consistency and a focus on sustainable lifestyle changes are key to achieving long-term success. By leveraging available resources such as therapy, support groups, and technology, individuals can find manageable paths toward their weight goals.